Undermeny

Coordinated health and care services
It has been a well-known problem for a long period of time that patients and users perceive the health and care services as being fragmented. The objective of this memorandum is to provide a patient- and user perspective of coordination, a perspective that emphasizes the fact that patients and users are participating and contributing agents in the coordination process. The memorandum does thus contribute to provide a broader perspective of the coordination problem in the health and care services and the social services.

View or download full report: Coordinated health and care services (pdf)
Summary
One of the great challenges for the health and care services and the social services in Sweden is to coordinate the services for patients and users. It is of great importance that the services are coordinated, for several reasons. Insufficient coordination does often lead to a worse experience for patients and users, in certain cases also to qualitatively inferior health care or care services. The shortcomings might also lead to higher costs, for example due to unnecessary repetitions of treatments or examinations.
When there is no coordination between the health and care services, a large part of the coordinating role is transferred to the patient, the user or her close relatives. If the health and care services do not at the same time take the ability and preferences of the individual to contribute to the coordination into consideration, there might be serious consequences. According to our estimates, there are about 1 million individuals in Sweden with several simultaneous needs who also have a reduced ability to coordinate their health and care services themselves. Moreover, this group is expected to grow every year as the population becomes older, which makes the coordination challenge even greater.
Altogether, the growing group of patients and users with several complex and related needs creates new demands on the health and care services, in particular as concerns creating coordinated health and care services with a focus on the individual. The operation is currently largely organised to meet patients and users with more clearly defined needs. Thus, we can see that the health and care services need to find new solutions in order to adjust to a more complex and extensive picture of needs.
The analysis takes an overall perspective och the health and care services and the social services
This report has a broad approach. The ambition is to consider the whole system for health and care services and thus identify overall structural challenges for achieving coordinated health and care services from a patient and user perspective. The objective of the report is to contribute with three new approaches to the coordination problem in a Swedish context:
- a description of what coordinated health and care services mean for patients and users.
- a framework to describe the needs for coordination of different groups, where the need includes the individual’s ability to contribute to the cooperation.
- an estimate of the size and use of resources for those groups that are included in the framework.
- a discussion of the main challenges that we see for creating more coordinated health and care services.
The report uses the term health and care services in order to describe all operations within the health and care services, elderly care as well as the social services. Many patients and users do, however, also have a number of other contacts with different authorities and operations in society. These also need to be coordinated within and between operations. For example, the services offered for vulnerable children and young people by the social services also need to be coordinated with school activities, as well as with different kinds of leisure activities. In accordance with the mission of The Swedish Agency for Health and Care Services Analysis, this report is limited to studying the coordination within and between the health and care services and the social services.
The analysis was carried out in the following way
The work can be characterised as exploratory. We started by trying to get a picture of the current level of knowledge, both at the national and international level. In order to get deeper insights into the core of the coordination problems, we have, together with the agency’s patient and user council, worked at trying to pinpoint how coordinated health and care services can be understood and interpreted from a patient and user perspective. In order to identify common challenges at the system level, we carried out 38 interviews with both local operation representatives and national experts, both from the health and care services and the social services. Then, we developed a theoretical framework in order to identify different general patient- and user groups and their need for coordinated health and care services. After that, we made a quantitative estimation of the size and costs of the groups.
Results
There are currently large shortcomings in the coordination of the health and care services
Both international and national studies show that patients and users are dissatisfied with the coordination in Swedish health and care services. Even if the problem is the same in many comparable countries, the insufficient coordination for Sweden is particularly evident from a patient- and user perspective.
Patient surveys within primary care do, for example, show that only slightly more than half of the patients feel completely secure with the coordination that is done by their contacts in the health and care services. A similar picture emerges in international comparisons of the health and care services: Only slightly more than 45 per cent of the patients in Sweden, for example, consider that doctors always or often assist in coordinating the health and care services from other operators. In this survey, Sweden performs the worst on this question as compared to other countries.
Those who work in the health and care services also experience that there is insufficient coordination. About half of the doctors in primary care do, for example, report that at least one of their patients has had problems in the last month due to the fact that there has not been any coordination in the health and care services. Similar shortcomings have also been observed in different ways in the social services.
It is estimated that about one million patients and users have a relatively complicated need for coordination while they also need extensive support in coordinating the health and care services
Our survey also shows that one million patients and users have complex coordination needs. Besides little ability to coordinate their own health and care services, the group is characterised by a high complexity in those services that are required. For these individuals, support that facilitates the coordination is of particular importance.
Individuals with complex needs do often need several health and care services from a large number of organisations and principals. If they also have limited abilities to be active and participate in their health and care services, the need for coordination becomes particularly large. In many cases, the total needs for these individuals can only be fulfilled by different agents coordinating their services.
Previous studies of the coordination challenges in the Swedish health and care services have often focused on specific patient and user groups within this general group, often the most ill elderly people. Our study shows that there is a considerably larger number of groups with similar coordination needs, for example individuals with serious mental and somatic comorbidity, individuals who have been subject to violence in close relationships, individuals with serious self-harm behaviour and individuals in a late palliative stage.
The need for coordinated health and care services differs between groups
The need for coordination differs between different patient and user groups. Thus, the challenges for obtaining a better coordination also differ. We have seen that there exists no general Swedish framework for discussing and analysing what the need for coordinated health and care services looks like for different patient and user groups. Swedish studies have almost always focused on an individual target group, often the elderly. Thus, there exists considerably less knowledge about several other groups but also about an overall perspective of how the need for coordination differs between different groups. The report also presents a framework for how the need for coordination can be described and analysed.
The framework takes its starting point in the assumption that groups with similar needs for coordination are close to each other on a scale that consists of the following two dimensions:
- The degree of complexity in the coordination of the individual’s needs for health and care services. Complexity here means how many of the services provided to the individual that need to be coordinated in relation to the organisational conditions that facilitate the coordination or make it more difficult.
- The individual’s abilities to participate in the coordination of his/her health and care services. This means how much help and support the individual needs from the health and care services in order to drive the health and care services process forward. For example, this is about making those contacts that are needed to satisfy one’s needs, to be a carrier of information and deal with part of the implementation on one’s own.
Based on its location in the framework, the Swedish population has been divided into five patient- and user groups:
- Group 1: Individuals with complex needs and little ability to participate in the coordination of their health and care services
- Group 2: Individuals who have recently become ill and need swift services from several agents and where the swift course of events affects the individual’s coordination ability
- Group 3: Individuals who are largely somatically healthy with little ability to participate in the coordination of their health and care services
- Group 4: Individuals with complex needs, but with good ability to participate in the coordination of their health and care services
- Group 5: Individuals with largely good mental and somatic health
Figure 1. Framework that describes the needs for coordinated health and care services for different general groups.
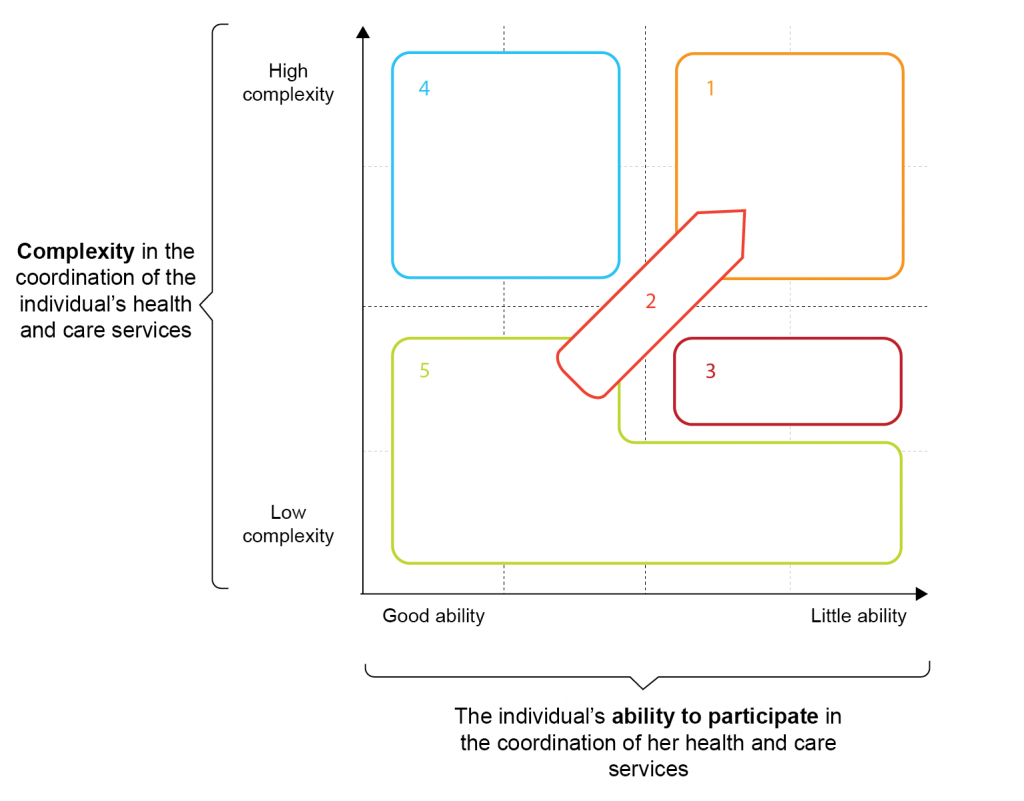
Those groups that are part of the framework are general enough to cover all patients and users in the health and care services. The objective is to be able to use the groups for an overall system analysis of the coordination problems, while they must also be sufficiently specific to be used as support for management and control of coordination and cooperation in county councils and municipalities.
Conclusions
There will be an increase in the need for coordination, mainly due to the growing group of patients and users with complex needs
The Swedish health and care services are facing a great challenge since patients and users with several simultaneous needs for health and care services constitute a continuously growing group. There are several reasons for this. The medical trend has led to individuals with chronic diseases living increasingly longer and having the time to develop more diseases. Alongside this trend, we can also observe an increasing specialisation in the health and care services, which leads to patients meeting a larger number of agents. Chronic diseases can now be considered as a normal condition among the elderly. In a previous study from The Swedish Agency for Health and Care Services Analysis it did, for example, emerge that 85 per cent of the population aged 65 or above did at least have one chronic disease and 66 per cent of these had two such diseases or more. And out of all elderly people who have home-care services or live in sheltered housing, the majority has one or several chronic diseases. The larger the number of chronic diseases, the larger is the need for contact with both the health and care services. Within medical care, there is also often a need for contacts with several different specialists besides the care centre where the patient is enrolled.
There are insufficient conditions for the staff in the health and care services to work in a more coordinated way
In order to achieve coordinated health and care services for patients and users, it is required that those professions that the individual meets from the health and care services coordinate their services. This might be about information sharing with each other or that they do, in practice, cooperate on a patient or user in their daily work. It is also those people who work closest to the patient and user who have the responsibility to see to it that the coordination works. At the same time, these professions work and act in a complex system. This system consists of different organisations and logistics for control as well as multifaceted objectives and requirements as concerns legislation and regulations, for example. The possibilities for the operations and the professions to coordinate their services are thus largely determined by the different conditions and incentives that the overall system will provide them with. We find that there are mainly four conditions that need to be fulfilled by the system for health and care services in order to obtain more coordinated health and care services:
- a patient and user oriented organisation culture that works for a common vision of the health and care services.
- overall system policies, laws and guidelines that provide conditions for coordination
- a formal coordination between organisations that creates conditions for coordination across the organisational borders
- administrative systems that facilitate coordination.
Based on our interviews and the overall analysis, it emerges that the health and care services system in Sweden faces considerable challenges as concerns all these issues.
- There is insufficient knowledge about what coordination is about and what each individual profession can achieve together with other professions through coordination. For example, the different professions in the health and care services do not always understand each other’s perspectives; what others can contribute and what can be achieved together.
- There is a lack of management and control as concerns the coordination issues. The operation managers find that it is difficult to lead and control in the direction of improved coordination. They have insufficient knowledge about what coordination means and how they can, in their role as managers, create conditions for coordination and what the results of this might be.
- Municipalities and county councils find it hard to create coordination contracts that have a real effect for patients and users. The contracts do, for example, tend to focus on a division of responsibility rather than on improving the coordination. Thus, for many questions, there is a grey zone where nobody takes any responsibility. There is often also a missing representative for patients and users when the agreements are made.
- Plans for care and coordinated plans do currently tend to be considered as a product of the drawing board rather than as a well-working plan for coordination. For example, it is common that, for various reasons, important agents do not participate when the coordination plan is drawn up. The plan does thus often have a limited effect on coordination.
- Primary care does not have sufficient conditions to take the coordinating role for the various care services that it is expected to have. The reasons for this can be traced back to the fact that primary care is, for example, characterised by an unclear definition of its mandate and its assigned tasks.
- The funding system does not create sufficient coordination incentives. Most remuneration systems do not specifically reimburse the coordination of services; coordination is rather often expected to be done within the regular funding. When coordination is not remunerated, such services runt the risk of being considered as a cost for the operation and are thus given lower priority.
- The current information structure of IT support does not provide sufficient conditions for coordination. Information about patients and users is seldom stored in such a way that it is easy for other people to use the information. The existing legislation does also prevent information sharing between county councils and municipalities. It makes coordination more difficult for patients and users with complex needs who are in need of support from both principals.
- There is no common view of what coordinated health and care services mean for patients and users
Coordinated health and care services is a term that is frequently used but there is no established definition. In the Health and Medical Services Act, there are clear requirements for coordination and continuity, but it is not exactly defined what is the exact meaning of coordinated health and care services. It is also clear that there is still a lack of coordination despite the legal requirements. One reason why the coordination is often insufficient is that there is no common view of what coordination is, something that has, for example, been emphasized in our interviews with operation representatives. In practice, it is difficult to coordinate with other agents if there is no common view of what is to be coordinated. This also constitutes an obstacle to making demands for and evaluating the coordination, both at the local and the national level.
In this report, we thus present a working definition of coordinated health and care services. The objective is to try to pinpoint what the term means from a patient and user perspective. We hope that this definition can contribute to, and facilitate, a continued discussion of both problems and possibilities for improvement in this area:
From a patient and user perspective, health and care services are coordinated when all activities are actively organised as a well-functioning entity from that individual’s perspective and where she is given the possibility, according to ability and preferences, to participate as an active contributor.
Our starting point is to particularly study what it means when the health and care services are coordinated from the patient and user perspective, i.e. coordination as a quality dimension for the final user. But the definition does also have consequences for citizens, organisations and the health and care services system as a whole. Coordinated health and care services can, in turn, be achieved through a number of organisational solutions, with varying extents of cooperation.
Continued work by the Swedish agency for health and care services analysis in this area
This report constitutes the initial work of The Swedish Agency for Health and Care Services Analysis in the area of coordination. On basis of this, largely exploratory, work, the objective is to, in the next stage, more specifically continue to work on possible solutions in order to achieve more coordinated health and care services. The framework of this report will constitute the basis for exactly defining principles for coordination and using these as the starting point to present examples for how a patient- and user adapted coordination can be achieved. Here, the frameworks make an in-depth analysis possible of how well different national and local coordination services are adjusted to the differences in the needs for coordination in different patient and user groups. In this way, we would like to illustrate how the current remuneration system, the organisation and the view of the health and care services need to be developed in order to meet the coordination needs of patients and users. We do, however, hope that already this report might be of use for more people who aim at working on coordination issues, at both the national and the local level.
View or download full report: Coordinated health and care services (pdf)
